The 6 Wagner Stages of Diabetic Foot Ulcers
Published on May 17, 2022
If you have diabetes, you may already know you’re at high risk of developing foot ulcers.
Diabetes seriously affects the feet. Peripheral neuropathy, one of the most common complications of high blood sugar levels, causes a loss of sensation in the feet, leading to wounds and sores staying unnoticed. Associated with poor blood circulation and a slow healing process, these wounds remain, get infected, and keep returning. They turn into diabetic foot ulcers.
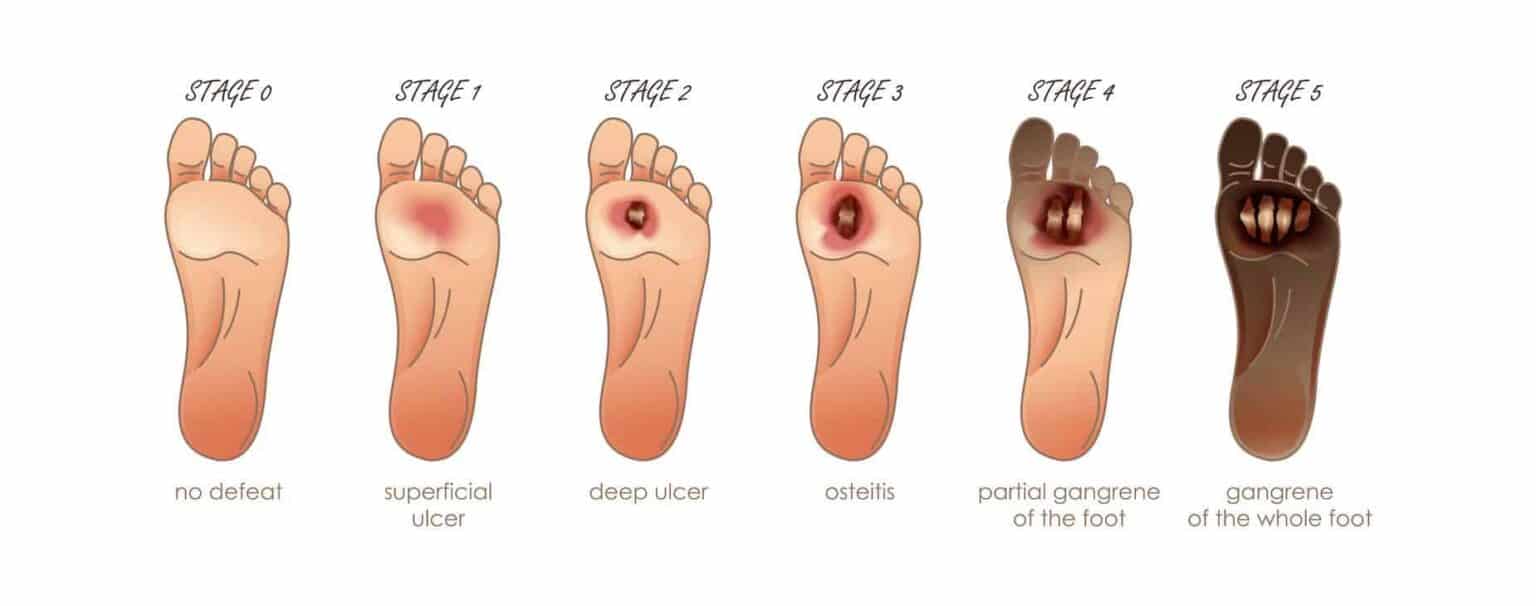
The Wagner classification system of diabetic foot ulcers allows healthcare professionals to grade the severity of a foot ulcer according to 6 different stages. Early and proper diagnosis of a diabetic foot ulcer may help prevent the amputation of a toe or a foot.
The Wagner Scale of Foot Ulcers
Classifying foot ulcer stages allows a better understanding of the patient’s condition and helps prevent or predict lower extremities amputations.
What is a diabetic foot ulcer?
An ulcer is an open wound or sore that does not heal and keeps returning. It most often affects people with diabetes, peripheral neuropathy, and circulation problems (neurotrophic ulcers).
Diabetic ulcers often look like a crater or a wedge on your feet. They’re usually minimal at the earliest stages (1 centimeter wide) but can quickly grow to the size of the entire foot if not treated. Diabetic foot ulcers might look yellowish pink, red, grey, or even black when the tissues are dead (necrosis, gangrene).
Foot ulcers can be found anywhere on the feet and toes, although they usually appear on pressure points. They can originate from tiny scrapes, cuts, blisters, or puncture on your skin. Diabetic peripheral neuropathy often causes a loss of sensation in the lower limb, which makes foot ulcers often unnoticed.
Neurotrophic ulcers can indeed be painless, but they lead to severe complications. Ulcers quickly get infected, and you may need to have part of a foot, or a toe amputated when the infection doesn’t go away. About 15% of people with diabetes get a foot ulcer at some point. In the United States only, about 75,000 amputations yearly are performed because of diabetic foot ulcers.
Wagner Classification of diabetic foot ulcers
The Wagner Classification system of diabetic foot ulcers was developed in the 1970s. It classifies foot ulcers according to 6 developing stages (from stage 0 to stage 5) according to the severity of the ulcer, its depth, as well as the presence of osteomyelitis (infection of a bone) or gangrene (necrosis, dear of tissues).
Wagner’s classification of DFUs is the most straightforward DFUs classification system. It does receive some critics, such as the fact that it does not adequately distinguish the different subtypes of diabetic foot ulcers and the spectrum of the infections.
Other classification systems for diabetic foot ulcers include the University of Texas Diabetic Foot Ulcer Classification System, the Diabetic Ulcer Severity Score (DUSS), and others.
The 6 Stages of Diabetic Foot Ulcers (Wagner)
According to Wagner, there are six stages of diabetic foot ulcer:
- Stage 0: no ulcer – the skin is intact, and there are no open lesions
- Stage 1: superficial diabetic ulcer affecting the outer layers of the skin
- Stage 2: deep ulcer – extended to ligament, tendon, joints, or deep fascia
- Stage 3: deep ulcer with bone involvement – access, osteomyelitis, or joint sepsis
- Stage 4: forefoot gangrene – dead tissues in the front of the foot or the heels
- Stage 5: whole-foot gangrene – the gangrene has spread to the entire foot
Diagnosing Diabetic Foot Ulcers at an Early Stage
An early diagnosis of diabetic foot ulcers helps prevent severe complications and amputations in most cases.
Remember that if you have diabetes, and even more so if you have been diagnosed with peripheral neuropathy, you may not feel the wounds on your feet. Inspecting your feet daily and checking for sores, blisters, irritations, cuts, and others is very important. It may help diagnose a diabetic foot ulcer at its earliest stage before it’s too late.
Always wear adequate, protective, and comfortable footwear. Diabetic shoes may help prevent most diabetic foot complications that could lead to ulcers.
If you notice anything unusual on your feet or feel any pain, wounds, or weird sensations, immediately seek your doctor’s advice.
People with diabetes should have their feet checked by healthcare professionals at least once a year during a proper diabetic foot exam.